World diabetics population, what is diabetes and Main types of diabetes
World diabetics population
Global diabetes prevalence is estimated to be 9.0% (420 million people).
Approximately 90 percentage are type 2 diabetes.
What is diabetes
Diabetes mellitus, commonly known as diabetes, is a metabolic disease that causes high blood sugar.
Main types of diabetes
. Type 1 diabetes
Type 1 diabetes is your immune system mistakenly attacks and destroys the beta cells in your pancreas that produce insulin. The damage is permanent.
. Gestational diabetes
Gestational diabetes is due to insulin-blocking hormones produced during pregnancy. This type of diabetes only occurs during pregnancy.
. Type 2 diabetes
Type 2 diabetes starts as insulin resistance.
Insulin resistance
In people with insulin resistance, the cells are unable to use insulin effectively. When the cells cannot absorb glucose, levels of this sugar build up in the blood.
Means for the same amount of circulating insulin, the skeletal muscles, liver, and adipose/fat tissue take up and metabolize less glucose than normal.
Prediabetes
This is the next stage of insulin resistance.
If the blood sugar levels are higher than usual but not high enough to indicate diabetes, doctors refer to this as prediabetes.
Diabetes type 2
The difference between prediabetes and diabetes type 2 is, how high the blood sugar levels are.
With type 2 diabetes, the body either doesn’t use the insulin properly or doesn’t produce enough insulin.
Main cause of type 2 diabetes applicable in general
. Obesity
Especially too much fat in the abdomen (belly) and around the organs, such as the liver, kidneys, pancreas, intestines, called visceral fat, is a main cause of insulin resistance that leads to type 2 diabetes.
(In the past, you have taken calories intake more than the burn)
. Inactive lifestyle/Lack of exercise
. Genetics factor on body shape
People who typically have apple-shaped bodies, meaning they have larger waists and carry a lot of weight around their abdomens are more likely to get. People having a pear-shaped body, that is, carrying more of your weight around your hips and having a narrower waist, doesn’t increase your risk of diabetes, heart disease and other complications of metabolic syndrome.
You can find out more about apple and pear-shaped bodies from the web images
General Type 2 diabetes pathway, Inflammation and Metabolic syndrome / Syndrome X
General Type 2 diabetes pathway
Obesity (excessive body fat)
Low grade inflammation in the white adipose (fat) tissue
Insulin resistance
Metabolic syndrome
Pre-diabetes
Diabetes type 2.
Inflammation
Inflammation is the body’s immune system’s response to an irritant. When you have chronic inflammation, your body’s inflammatory response can eventually start damaging healthy cells, tissues, and organs.
Chronic inflammation has been linked to certain diseases such as heart disease or stroke, and insulin resistance, certain type of cancers and metabolic dysfunction.
Metabolic syndrome / Syndrome X
Metabolic syndrome is a cluster of conditions that occur together, increasing your risk of heart disease, stroke and type 2 diabetes. These conditions include increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels. MetS is a state of chronic low-grade inflammation with the profound systemic effects.
Metabolic syndrome is present if three or more of the following five conditions are met.
The five risk factors are:
. Increased blood pressure (Insulin resistance, NAFLD – Nonalcoholic fatty liver disease)
. High fasting blood sugar levels (insulin resistance)
. Excess fat around the waist (Abdominal obesity/central obesity/belly fat) (Insulin resistance)
. High triglyceride levels (NAFLD, Insulin resistance)
. Low levels of good cholesterol, or HDL. (NAFLD, Insulin resistance)
Causes,
Overweight and obesity
An inactive lifestyle
Inflammation in the white adipose tissue.
Complications,
Insulin resistance and type 2 diabetes
Non-alcoholic fatty liver disease
Cardiovascular disease
Stroke
High blood pressure
Kidney disease
Some types of cancers
Arteriosclerosis, hardening of the arteries or thickening of the artery walls, which increases the risk of stroke, heart attack and heart disease.
Development of vascular (vessels which carry blood) complications, high blood sugar, retinopathy (vision), nephropathy (kidneys), and peripheral neuropathy (nerves outside of the brain and spinal cord, peripheral nerves) problems.
Preventing or Reversing metabolic syndrome, Action of insulin on the body, Insulin resistance, Insulin resistance and vicious circle paths, Explanation of insulin resistance in the target tissues/organ and Insulin sensitivity
Preventing or Reversing Metabolic syndrome
You can prevent or reverse metabolic syndrome by making lifestyle changes, like losing weight, exercising regularly, eating a healthy, balanced diet to keep your blood pressure, cholesterol and blood sugar levels under control.
Having metabolic syndrome can increase your risk of developing type 2 diabetes. If you don’t make lifestyle changes to control your excess weight, you may develop insulin resistance (or you already have), which can cause your blood sugar levels to rise. Eventually, insulin resistance can lead to type 2 diabetes.
Action of insulin on the body
Insulin helps control blood glucose levels by signalling the liver, muscle and fat cells to take in glucose from the blood. Insulin helps the cells absorb glucose, reducing blood sugar and providing the cells with glucose for energy.
If the body has sufficient energy, insulin signals the liver and muscles to take up glucose and store it as glycogen (storable form of glucose).
When blood sugar levels are too low, the pancreas releases glucagon (a hormone). Glucagon instructs the liver to release stored glucose, which causes blood sugar to rise.
Pancreas
Pancreas is an organ that helps in digestion and blood sugar control.
Insulin resistance
Means, for the same amount of circulating insulin, the skeletal muscles, liver, and adipose tissue take up and metabolize less glucose than normal.
And the result is you will find both more glucose and more insulin circulating in the blood, when compared to a normal person, instead of glucose being absorbed by the body.
Insulin resistance and vicious circle paths
Path 1
Excess body fat leads to high insulin resistance.
High insulin resistance leads to excess body fat.
Path 2
Chronic inflammation (in the white adipose cells) leads to high insulin resistance.
High insulin resistance leads to chronic inflammation (in the white adipose cells).
To reverse this circle, you need to reduce inflammation in the white adipose tissue and reduce body/belly fat.
Explanation of Insulin resistance in the target tissues/organ
. Insulin resistance in skeletal muscle
In skeletal muscle, insulin resistance is manifested as a decrease in glucose transport and a decline in muscle glycogen (storable form of glucose) synthesis in response to circulating insulin. And reduced usage of glucose by muscles.
Glucose uptake into muscle is essentially insulin dependent and muscle accounts for about 60–70% of whole-body insulin mediated uptake.
Your muscle stores around 1200 Cals of glucose in the form of glycogen for the day today needs, especially for heavy usage. This is not used properly. Also, less glucose is burned by the muscles each day. When you eat food and it is digested, the uptake of glucose is very less.
In the early stages of development of type 2 diabetes, impaired glycogen synthesis in muscle is the primary defect responsible for the insulin resistance.
Skeletal muscle insulin resistance is the primary defect in type 2 diabetes.
. Insulin resistance in the liver(hepatic)
In the liver, insulin fails to suppress gluconeogenesis (generation of glucose from non-carbohydrate carbon substrates such as lactate, glycerol, and glucogenic amino acids).
The normal function of liver, in the fed state is, to uptake glucose from digested carbohydrates and synthesis glycogen and store it for later use. When the blood glucose levels go below the lower limit, after the digested food is used, glucose is to be released in the blood stream.
Explanation
For a diabetic individual,
In the diabetes state, insulin action is decreased at the liver and leads to increased hepatic gluconeogenesis and, increased glucose release to the circulation, reduced glucose uptake into peripheral tissues, and increased blood glucose levels.
That is your liver is not up taking glucose and making glycogen in fed state and instead, always releasing glucose in the blood.
For a normal, non-diabetic individual,
Liver both stores and manufactures glucose depending on the body’s need.
During the fed state, glucose is taken and stored in the liver as glycogen.
In the fasted state, the liver secretes glucose through breakdown of glycogen (glycogenolysis that is breakdown of the molecule glycogen into glucose) and releases to blood.
During prolonged/long fasting, hepatic (liver) gluconeogenesis is the primary source of endogenous (originates within) glucose production.
. Insulin resistance in adipose(cells) tissue/ fat cells (that is in the fat cells where the excess food intake is converted to fat and stored in the form of triglycerides)
In adipose tissue, insulin resistance is manifested as impaired insulin-stimulated glucose transport/intake, as well as impaired inhibition of lipolysis (breakdown of fats) in obese people (too much of stored fat in those people have, is released without inhibition. Normally when the blood insulin is high, stored fat cannot be released).
For the amount of circulating insulin, glucose entry is impaired in fat cells.
Insulin sensitivity
Insulin sensitive people will require smaller amounts of insulin to lower blood glucose levels.
If you have insulin resistance, you have low insulin sensitivity. Conversely, if you are sensitive to insulin, you have low insulin resistance. While insulin resistance is harmful to your health, insulin sensitivity is beneficial.
Reversing type 2 diabetes and IN SUMMARY
Reversing type 2 diabetes
You need to improve the insulin sensitivity in all the three areas namely muscle, liver and adipose tissues.
. How to increase muscle insulin sensitivity
. Use muscles to burn calories by exercise/muscle contraction or though physical activity every day.
. Deplete the stored glycogen, triglycerides and other lipids by exercise/CR or by both from the muscles.
(CR-Calories restriction)
.(You normally can store up to 1650 calories in muscles).
. Build more muscles.
. How to increase hepatic(liver) insulin sensitivity
Taking Metformin (treatment medicine).
Reducing storage of triglycerides and other lipids in muscles every day.
Reducing accumulation of liver fat.
Reducing total abdominal, that is truncal (belly and above the belly), both subcutaneous and visceral fat located near several vital organs, including the liver, pancreas, kidneys, stomach, and intestines.
(Excess visceral fat primarily increases gluconeogenesis movement. Excess visceral fat is fed in to the liver. Both visceral fat and liver fat are associated with hepatic insulin resistance).
Need to reduce at least 7 to 9 kg of weight to have hepatic insulin sensitivity to be under control. Or, bring down the body fat percentage to17-21 for men and 25-29 for women.
. How to increase adipose tissue / fat cells insulin sensitivity
Improvements in hepatic(liver) insulin sensitivity
Improvements skeletal muscle insulin sensitivity
Reducing total body fat
Improvements in full system (in all three areas) glucose tolerance.
IN SUMMARY,
The act of reducing the insulin resistance hence reversing type 2 diabetes is increasing the insulin sensitivity in muscles, liver and adipose tissue by,
Depleting (may not be to zero levels) stored muscle glycogen, triglycerides and other lipids every day
Using muscles to burn calories
Reducing accumulation of liver fat and visceral fat
Reducing total abdominal(belly) fat
Reducing total body fat.
All the above can be achieved by,
Calories restriction (CR)
Exercise
Building more muscles.
Better understanding of the type 2 diabetes
Managing diabetes means just
. Improving Muscle sensitivity on day today basis.
Controlling diabetes is actually
. Reversing Hepatic/liver sensitivity
. Approximately loosing 7 to 9 kg of your weight
and body fat percentage should be 17-21% for men and 25-29% for women.
Reversing diabetes is improving,
. Total adipose sensitivity
. Removing most of the abdomen fats, all the ectopic fats and removing most of the visceral fats, especially in the liver and pancreas no fats other than the required essential fats, making pancreas fully functional and capable of secreting enough insulin to meet the demand
. Approximately your body fat percentage should be of 13% for men and 22% for women
You cannot spot reduce stored fats. By this time, you would have lost a big amount of subcutaneous fat also.
The above numerical values/figures are only approximate and a guess, and can vary with population.
Digestion, energy, storage and Fat storage
Digestion, energy and storage
When you eat food, it is digested and your body turns food you eat into nutrients, it uses for energy, growth, and cell repair.
All the muscle cells cardiac, smooth, and skeletal, mainly use carbohydrates and fats for energy. Muscle cells burn calories and produce energy for the organs or the body.
Digested protein is used for building muscles, excess protein is either used for energy, stored as triglycerides or excreted.
If you eat more than the body requirement, it is stored as fat in adipose tissue(cells) as triglycerides.
Fat storage
White fat, or white adipose tissue (WAT), stores your energy in large fat droplets that accumulate around the body. The accumulation of fat helps keep you warm and by literally providing insulation for your organs.
White adipose tissue (WAT) is composed of,
. Subcutaneous WAT and
. Visceral WAT.
Subcutaneous WAT(SAT)
SAT (Subcutaneous white fat) represents 80 percent of all fat tissue in people and it is stored in the hips, buttocks, arms and thighs. Subcutaneous fat is located directly under the skin all around the body and also in the outer abdominal wall. You can squeeze or pinch teem.
When energy intake (food) is too much, over the time, the ability to store calories in subcutaneous white fat, ‘spills over’ into organs that are not specialized for storing fat, such as the liver, pancreas, heart and muscle. This will lead to ectopic fat.
Ectopic fat
Ectopic fat is storage of fat in tissues other than adipose tissue, that normally contain only small amounts of fat, such as the liver, skeletal muscle, heart, and pancreas. Ectopic fat can interfere with cellular functions and hence organ function and is associated with insulin resistance, type 2 diabetes, cardiovascular diseases and atherosclerosis. That is, it increases metabolic risk factors and vascular diseases.
VAT (Visceral fat)
VAT (Visceral fat), also known as “belly fat,” is the white fat that’s stored in your abdomen and around all of your major organs, such as the liver, pancreas, stomach, kidney and intestines.
Visceral adipose tissue can’t always be seen directly and hangs around your organs, making it more dangerous to your health and more strongly associated with metabolic syndrome and diabetes compared to subcutaneous fat. About 10 percent of all body fat is visceral.
BAT (Brown fat)
BAT, Brown fat, or brown adipose tissue, stores energy in a smaller space than white fat. It has more mitochondria, when brown fat burns calories, it creates heat to help maintain your body temperature in cold conditions.
Brown fat is found in neck, shoulder blades, spinal cord etc.
Mitochondria
Mitochondria are often referred to as the powerhouses of the cell. They turn the calories we take from food into energy that the cell can use. All the cells except red blood cells have mitochondria. Heart, liver and skeletal muscle cells have many mitochondria per cell. In white adipose cells not so many.
For better understanding of the location of various fats SAT, VAT, BAT and Ectopic fat with images, search in individual fat name on web search on images.
Main reasons for diabetes (science), Why diabetes has high fasting blood sugar levels; Effect of intake of carbs, protein and fats on blood sugar and blood insulin
Main reasons for diabetes (science)
Excess visceral and ectopic fats,
Inability to store the additional fats (excess calories) by the circulating insulin,
Calories are not burned every day or less physical/muscle activities,
Liver always produces sugar and releases in to the bloodstream,
Less muscle to body fat ratio (less muscles and more visceral and ectopic fats).
Why diabetes has high fasting blood sugar levels?
Increased gluconeogenesis in the liver of patients with type 2 diabetes is considered a major contributor to hyperglycaemia and subsequent diabetic organ damage.
In type 2 diabetes with fasting hyperglycaemia (>140 mg/dl, 7.8 mmol/l), an excessive rate of endogenous (by the liver) glucose production and glucose output is the major abnormality responsible for the elevated fasting plasma glucose concentration.
Effect of intake of carbs, protein and fats on blood sugar and blood insulin
Blood sugar from macros/macronutrients
Normally only carbohydrates spike your blood sugar levels.
Protein has a minimal effect on blood glucose levels with adequate insulin. However, with insulin deficiency, gluconeogenesis proceeds rapidly and contributes to an elevated blood glucose level.
Fat we eat does not directly raise our blood sugar levels.
To keep your blood sugar low, replace the intake of carbohydrates with good balanced fats. Too much of protein is not good for your kidneys.
Blood insulin from macros/macronutrients
Insulin is required for carbohydrate, fat, and protein to be metabolized.
Requirements of insulin in descending order is as follows:
Carbohydrates, some of the vegetables protein like legumes of big sizes, curd/yogurt (greater than) > animal protein & some of the vegetables protein legumes of small sizes, > nuts > oils/fats.
Oils and fats don’t spike blood sugar and insulin or is minimal.
In general,
Carbohydrates spike both blood sugar and insulin in the blood in high levels.
Protein normally does not spike blood sugar provided if your body produces enough insulin. Protein metabolism requires medium amount of insulin compared with carbs.
Fats/oils do not spike blood sugar and do not require much insulin.
For a diabetic, carbohydrate is to be replaced with balanced fats and adequate protein.
Calories storage and usage
Calories storage
Energy/calories reserves of a 70kg man calories(kcal),
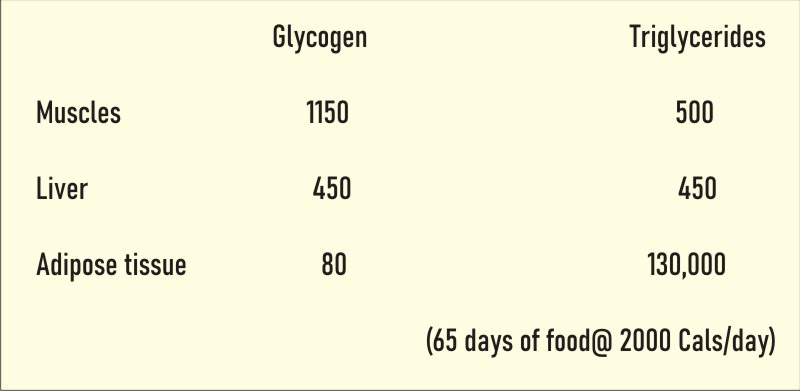
. Glycogen – storable form of glucose
. Triglycerides – storable form of fat.
Glycogen and Glucose
. Glycogen is stored in the liver and can be released back into the blood stream
. In Muscle, where it can be converted back to glucose but mainly used by the muscle
. Each gram of glycogen is stored with at least 3 g of water
. Adipose cells don’t store much water, they expand or shrink in size along with both fat and water. Very less glycogen is stored.
. Athletes/Body builders can burn glycogen reserves in about 2 hours. It takes approximately 24 hours to refill the depletion, post high carbohydrate meal.
. On a blood volume of 5 litres, only four grams of glucose circulates in the blood of a person weighing 70 kg. This glucose is critical for normal function in many cell types.
. In accordance with the importance of these 4 g of glucose, a sophisticated control system is in place to maintain blood glucose constant.
Storable form of calories
As glycogen 1680 Cals
As triglycerides 130,000 Cals (65 days of food@ 2000 Cals/day).
Usable form of calories
. Glucose (glucose or breakdown of glycogen)
. Fatty acids (fatty acids or breakdown of triglycerides)
. Ketone bodies.
Ketone bodies are produced by the liver from the stored fat from fatty acids when the insulin level is low, during periods of low food intake, carbohydrate restrictive diets, starvation, prolonged intense exercise and alcoholism.
Also produced when in low carb, high fat (Keto) with a normal calories intake or CR keto diet.
For a type 2 diabetic to create such a condition and bring down low insulin level is, you need to deplete around 1500 calories that is stored as glycogen in muscle and in liver by calories restriction (CR)or burning through exercise or by both.
This will increase muscle insulin sensitivity, that is when you eat carbohydrates you have created a space for glucose uptake/storage.
By burning the food under digestion or stored glycogen plus triglycerides and other lipids from muscles regularly by exercise is another way to increase your muscle insulin sensitivity. This is not by CR.
As long as you are in the state of diabetes, the stored body fat burn will occur only after about 4 days post depletion of stored glycogen, if you deplete 500 Cals per day by exercise or by calories restriction (CR).
This will be the case when there is a break in calories restriction (CR)/exercise plus of excess calories input and if you come back for fat loss program after a few weeks.
